How to Create Supportive Relationships When Facing Chronic Pain and Fatigue
LISTEN ON YOUR FAVORITE PODCAST PLATFORM
Show Notes
Jenelle Coolidge discusses the impact of chronic pain, health issues, and fatigue on relationships. Learn what you can do for, how to enact self-compassion, and build supportive relationships while managing chronic conditions.
05:44 Specializing in Eating Disorders and Chronic Illness
09:37 Understanding Chronic Pain and Fatigue
11:06 The Mind-Body Connection in Chronic Illness
15:53 Challenges in Relationships with Chronic Illness
25:27 Self-Care and Self-Compassion Strategies
30:50 Misconceptions About Chronic Illness
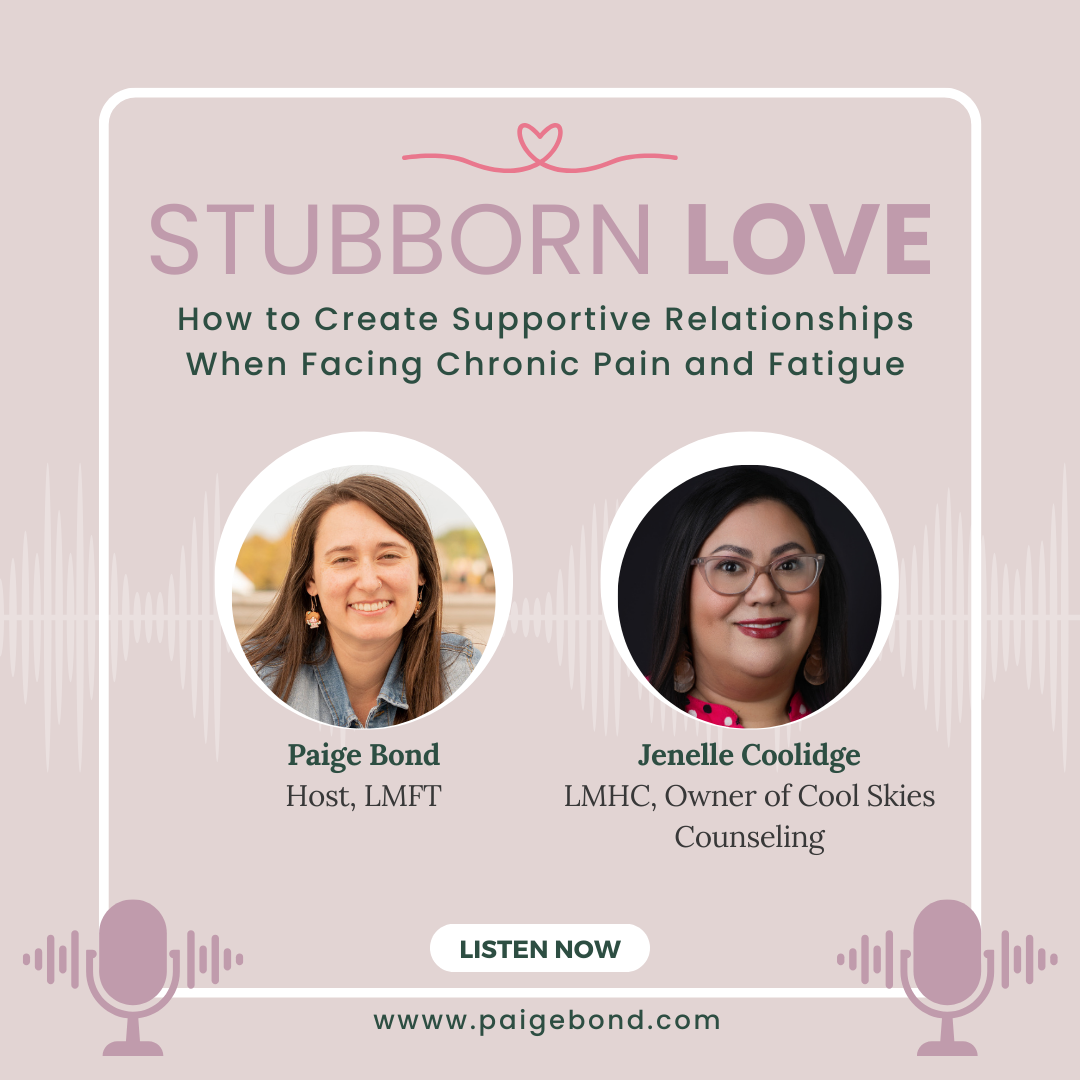
Jenelle Coolidge is a Licensed Mental Health Counselor and Certified Eating Disorder Specialist (CEDS). She specializes in eating disorders, chronic illness, trauma and mood disorders. Jenelle has a vast level of experience working in different mental health settings from Psychiatric hospitals, Residential facilities, Mental Health Clinics, Community Mental Health, and Private Practice and before as a mental health nurse. She also self-published My Body Liberation journal. When not working she enjoys gaming, movies, reading, and anything having to do with marvel.
Connect with Jenelle Coolidge
My website is www.coolskiescounseling.com
Facebook @coolskiescounseling
https://www.linkedin.com/in/jenelle-c-16a02410b/
Connect with Paige Bond
Website: https://paigebond.com
Website: https://SweetLoveCounseling.com
Paige Bond specializes in helping individuals, couples, and intentionally non-monogamous partnerships feel grounded, confident, and connected in their love life. She is also the founder of Sweet Love Counseling providing therapy in CO, FL, SC, and VT. Paige loves educating people about relationships through being the host of the Stubborn Love podcast, hosting workshops, and speaking at conferences.
Free Jealousy Workbook:
http://www.paigebond.com/calm-the-chaos-jealousy-workbook-download
Free People Pleasing Workbook:
https://www.paigebond.com/people-pleasing-workbook
Attachment Dynamics Workshop:
https://www.paigebond.com/attachment-dynamics-workshop-sign-up
Disclaimer: This podcast and communication through our email are not meant to serve as professional advice or therapy. If you are in need of mental health support, you are encouraged to connect with a licensed mental health professional to receive the support needed.
Mental Health Resources: National Suicide Prevention Lifeline: 1-800-273-8255SAMHSA’s National Helpline: 1-800-662-HELP (4357)Crisis Text Line: Text HOME to 741741 for free, 24/7 crisis counseling.
Intro music by Coma-Media on pixabay.com
Transcript
(generated by AI - please excuse errors)
[00:00:00] Paige Bond, LMFT: Welcome to the Stubborn Love Podcast. I'm your host, Paige Bond. I'm a Gottman and attachment trained, solution focused marriage and family therapist. I specialize in helping folks design and build their dream relationships through structured therapy and resources. And also use modalities that go beyond traditional talk therapy, like accelerated resolution therapy and psychedelic assisted psychotherapy.
School didn't teach us how to be good at love, so I created the Stubborn Love podcast to help you navigate it. Every episode has actionable tips that will help you create a happier, healthier, and more fulfilling life with the people you love. Join me on this journey of love and learning for the stuff they didn't teach you in relationship school.
Well, hello listeners. Welcome back to another episode of stubborn love. today we have a very special guest, a local therapist in my community. Jenelle Coolidge is gonna be talking today about chronic pain, chronic health issues, and fatigue.
I think all of us either have experienced or know someone who has experienced these things, and I think they can really have a drastic impact on relationships and how we relate to each other. So I'm really excited for this topic today, Jenelle. We have so much to dive into but before we do any of that, can you introduce yourself to the listeners, talk about who you are, what you do, and we'll get this show rolling.
[00:01:37] Jenelle Coolidge, LMHC: Thank you, Paige. I'm really excited to be able to come on as a guest of yours, I am Jenelle. I'm a licensed mental health counselor. I primarily specialize in eating disorders, chronic pain, chronic illness, mood disorders, trauma. All of those are my passion. Uh, but before becoming a therapist, I used to be a nurse, so there's where my medical interest came.
[00:02:08] Paige Bond, LMFT: I did not know that. Okay. Tell me how you went from nurse to therapist. This is interesting.
[00:02:16] Jenelle Coolidge, LMHC: of course I became a nurse because a lot of my family was like, okay, you're gonna make more money here. Like, you know, the usual, and although I really did have an interest in like medical and health, when I would take jobs as a nurse, I couldn't like stick with them 'cause I couldn't, you know, it took a while to figure out like, maybe this is not for me.
The only one that stuck around the longest was when I worked as a mental health nurse and I started seeing, oh my God, I like mental health
[00:02:48] Paige Bond, LMFT: the most. Oh, okay. That's the fast track to the therapy world then?
[00:02:53] Jenelle Coolidge, LMHC: yes. That's what like started my path of maybe what I really wanna be is a therapist.
[00:02:59] Paige Bond, LMFT: Mm-hmm. So at first you were more medical focused and then you started working in mental health. Is that an inpatient hospital or something that you were working in? Or what was the setting like?
[00:03:09] Jenelle Coolidge, LMHC: So I started at a state hospital, psych state psych psychiatric hospital in Washington State.
[00:03:17] Paige Bond, LMFT: Oh, okay.
All right. And so that's usually people who are experiencing like really extreme mental health issues, suicidal ideation or psychosis I'm assuming, or what's the run of the mill?
[00:03:30] Jenelle Coolidge, LMHC: Yeah, absolutely. you know, unfortunately when, by the time they get to the state hospital, these are people who have like involuntary commitment to, up to like 180 days,
And like long-term, severe psychopathology like schizophrenia, schizoaffective, bipolar, psychotic features, um, different personality disorders, lots of self-harm, lots of suicidal ideations. So these people, like before they get here, they've already done multiple like baker acts. They've done like outpatient, ,PHP, IOP.
Kind of like, almost like the last stop, basically.
[00:04:10] Paige Bond, LMFT: Yeah. Oh, I'm sure that you saw so many different people come through, and I'm sure it was a lot of work to be able to show up every day and, and, make sure that everybody is getting taken care of. You said that that was kind of like a, what precipitated you becoming a therapist.
So can you talk about your, your journey, how that shifted for you into the therapy world?
[00:04:36] Jenelle Coolidge, LMHC: Yeah. 'cause I just noticed anything involving nursing skills were just like low interest for me, but just like passing out the psychiatric medications, talk about side effects, talk about how they're doing mentally, their behavior.
Like all that was always so interesting to me. and I just wanna do more than just med passes or the injections that, you know, they don't want to do, but their court ordered. I was just like, I just wanna do something a little bit more than that.. then I had my own personal therapist and just noticing the difference that they made in my life I was like, why don't I just do this? You know? Go for it. this is obviously something that's like brewing and passionate. A passion of mine, so I, I decided to make the change.
[00:05:25] Paige Bond, LMFT: Oh, I love that for you. and especially that you had a good experience with a therapist that kind of sparked this even more in you.
I think a lot of times why we get into the field is either because of the shit that we've gone through or the shit that someone else has helped us through and we're like, we wanna repay the favor, or something like that. so thinking about that, starting your, your journey, you're now in private practice as a therapist and, and you know, you mentioned specializing and eating disorders and the chronic pain, health and fatigue issues.
Can you talk about how you started, moving towards that specialty?
[00:06:03] Jenelle Coolidge, LMHC: Yeah, absolutely. I was always interested in eating disorders because I am recovered. there's been a history of struggling with body image. Like I can remember as young as like you 11 or 10, like just, really looking at the mirror and checking and like wanting to be smaller and just through my own personal work and recovery, I was able to be like, this is where I really want to specialize, because it's really a passion of mine to help people get to recovered stage. And just because eating disorders also has so much, like medical aspects to it is also really interesting to me because I, I still do like the medical world, so I love that I get to still combine mental and medical with eating disorders.
[00:07:00] Paige Bond, LMFT: And if I'm not mistaken, you can correct me if I'm wrong 'cause this is, you know, your jurisdiction, but isn't eating disorders one of the most dangerous or deadliest mental health diagnoses that we can have out there? Like it has the highest mortality rate?
[00:07:17] Jenelle Coolidge, LMHC: Yeah, I've definitely heard of it. I think what I've always heard is like the opioid is like, like the deadliest and then eating disorders is Yeah. Right after that, It's, it's pretty dangerous.
[00:07:28] Paige Bond, LMFT: Yeah. Yeah. And thank you for sharing, that personal piece about you. Like I, I even got a little bit of goosebumps as, as you were talking about your own personal story because I think.
All of us struggle with body image. I, I remember looking at myself or having people tell me that I wasn't looking the right way. That, you know, we're supposed to look and be and how we have to fit in all these boxes and, I, I think. This is something that a lot of people go through. And so, you specialize in eating disorders and the chronic pain and health, issues.
Talk about your journey moving towards those chronic, places.
[00:08:09] Jenelle Coolidge, LMHC: Yeah, absolutely. so besides the interest in the medical world and just. Still wanting to put it into like my work now. I've also have like lived experience with, a chronic illness. And just remember, I think it was like, yeah.
Mid twenties and late twenties, just being like, I'm always tired, or my joints always hurt, or I'm always having stomach issues and kind of being dismissed by family and like, oh, you're too young for that.
[00:08:43] Paige Bond, LMFT: Mm-hmm.
[00:08:44] Jenelle Coolidge, LMHC: Even though chronic illness, did run in my family. 'cause I have, um, Crohn's colitis and stomach issues like that run in my family.
It was like there's no need to like dismiss me. I mean, it's genetic.
[00:08:59] Paige Bond, LMFT: Yeah.
[00:08:59] Jenelle Coolidge, LMHC: it just combining that with like recovering from an eating disorder and body image issues can be like so frustrating 'cause you're like, not only do you have to make peace with appearance, but also peace with the level of functioning it can. Do you know what I mean? It could be
[00:09:17] Paige Bond, LMFT: so frustrating too, especially when you might wanna do more or push past than what your body is telling you not to do I'm sure.
[00:09:26] Jenelle Coolidge, LMHC: yes 'cause obviously the younger you are, the more busy the mind is and wants to be all over the place, but sometimes the body doesn't align with it, so it's like a battle.
[00:09:36] Paige Bond, LMFT: Yeah. So for those who aren't familiar, and for me as well, can you actually put a definition, in the simplest terms that you can of what chronic pain health issues or chronic fatigue actually is like, how would you tell someone about it? Like if I were coming to see you and you're talking about it in, a session with someone, what is that?
[00:09:58] Jenelle Coolidge, LMHC: Absolutely. So going back to my years in the past of school,do rewind. basically I learned that like short term pain, is, or like a illness, it would be like no more than like six months. And then after that is when it becomes chronic, is what I can remember. there's also like an injury, right?
damage, structured damage that requires attention now, right? Then is after the attention now, right? Where tissue or whatever you're being worked on by the doctors and treated after a certain amount of time, if you still keep complaining about fatigue and pain and other issues, is when you start moving a little bit more chronic and it can become complicated because then the reasons for this can be many things.
[00:11:06] Paige Bond, LMFT: It could be Mainly, I would say 'cause of the mind body connection, mental health trauma, right? All that, that gets trapped in the body, that sometimes does increase flare ups, more pain, more fatigue. It's just so tied together that's why I think it's so important for the, the medical world to collaborate more with the mental health, Yeah, I was actually wondering about that because it is mind blowing how much of the mind body connection there is, like if you're stressed out or if you're having tough mental health days, they are so interconnected and I wonder how often in the medical field this intersection gets dismissed and just "no, you know, here take these anti-anxiety pills that should fix this flare up or something for you."
Or, or like, it really isn't being addressed at the root and I'm wondering what's your experience with that?
[00:12:11] Jenelle Coolidge, LMHC: Yeah, I mean, from the, from clients that I've worked with, there's so much medical trauma involved of not being seen or validated and almost like this. It's kind of like contradicting. It's like I want a diagnosis, I want a label.
Not because they wanna be sick, but because they'll finally be seen or understood. Less confusion and like even identity, Mm-hmm. So, and even from lived experience, just like the whole, like back and forth from one specialist to another specialist to so many appointments, they're so time consuming.
there's so much that goes into it thatThe client or the patient is not really thought as a whole, you know, like this is a, a person with a life,
[00:12:59] Paige Bond, LMFT: Yeah. And especially when dealing with insurance companies, we're all just numbers. I won't even get started on that 'cause I'll get too riled up.
gosh, like you talk about how you need at least six months. and then moving towards the year mark for this to be really chronic. I mean, that's exhaustingfor you to be taken seriously. I'm sure you're just passed around poked and prodded and just not getting answers.
I mean, I'm sure there's plenty of listeners who have had this same experience and, and what do you say to, to people like that who have been invalidated to, from the medical community? Like how can you support them and help them advocate for themselves and feel, like that, that there's still hope?
[00:13:41] Jenelle Coolidge, LMHC: Yeah.
Yeah. I mean it's, it's hard because when you're first being assessed to see like what's going on there is gonna be a couple of visits, right? Because they're trying to rule out things like, what's going on? "Is it this disease? Is it this, is it that?" Right? And I, it's just. People can get tired and fatigue, and so just really making sure that you're taking care of yourself with self care and leaning on to like support with a community to lift your spirits. Because it sometimes does take a while for doctors. Like they might need to do a bunch of tests, right? To make sure they are properly ruling out things and they're not missing stuff, right? It's so important to be properly checked and monitored. as far as advocating, like sometimes it's just really helpful.
You know, take a little, like a little mini journal of your health and like really write down what your symptoms have been. just like clinicians onset, duration, you know what I mean? The more detailed you can be with a provider, the more they can help you. Like if you tell them Pain started this for this amount, pain feels like that.
Like that's how clinicians think, especially in the medical world. The more data, the more specific you can be, the more they're like, "okay let me act on this."
[00:15:09] Paige Bond, LMFT: Yeah.
[00:15:09] Jenelle Coolidge, LMHC: it's extra work and it's frustrating, but sometimes like the way you communicate, you know, there's a difference.
Like the provider's almost like, oh, okay, you know, there's like more like energy to work or something. I don't know.
[00:15:25] Paige Bond, LMFT: yeah. Well, they need it so that they can do something with it. So that makes sense. But that also has to be probably exhausting or like really hard to do and remember to document all of these things like I'm sure.
You know, someone living with these chronic conditions like you're trying to live your life, and so then it gets interrupted by this pain occurrence or whatever the incident is, and then you have to take your attention away from that to do this task. I'm wondering how these chronic conditions interrupt, people's daily lives and interrupt their, dynamics with other people in their lives.
Can you speak to that?
[00:16:05] Jenelle Coolidge, LMHC: Yeah, it's definitely can become discouraging and exhausting, for a person to track every single time. So honestly, like just doing the best that you can, bringing in the self-compassion, bringing the self-care. And then when it comes to like relationships, like it's so important to have like a a good community, a good group, or if we're even talking about like intimate, partners and stuff, it's really important for the partner to also get educated on what's going on. because a lot of times the other person feels like a burden. they feel sad or ashamed that they have to, or guilty that they have to ask for so much more help.
And they're like, I'm, they have to pick up so much because I can't do stuff. And maybe that partner can like communicate one-on-one about like, no, you're not a burden. Like, kind of a little bit about like, "I love you, I want to support you." It's just making sure like that I feel statements are really like.
Loud and clear on both parties so that no one is feeling like they're not being heard or seen,
[00:17:24] Paige Bond, LMFT: Yeah. Now, on the other side of things, 'cause like that's best case scenario where you have a partner who is really willing to put in that extra effort and, show up in the relationship the, the way that the other needs.
But have you seen it go wrong where the partner who's not faced with the chronic conditions, they're not willing to help. they do think that this person is a burden. do you get people coming to you and saying like, "no, they're, they're not willing to, to work with me on this. And like, I feel, I still feel like a burden because their actions are basically telling me, that I am."
do you see that in your work with people?
[00:18:02] Jenelle Coolidge, LMHC: I have sadly seen that, where the partner has been so, like, like even if they don't say "you are a burden," their behaviors, say it loud and clear, where,the other person's having to worry about like if they're gonna have enough money to pay for their meds, right?
Mm-hmm. Worried about what kind of job they can do because their other, like, their partner's like, "no, you need to take care of that financially on your own." it's very much you, your problem type of message. And so just to see the pain and struggle and hopelessness in that person is really sad, you know, because that person really needs to get supported at this time. Like basic things, such as like if they need to be worried about meds and health and insurance, like that's just like basic,
[00:19:05] Paige Bond, LMFT: Yeah.
[00:19:05] Jenelle Coolidge, LMHC: Then we move on to like actual emotional support, so if their basics cannot be taken care of, like we're talking about extra trauma here, building.
[00:19:17] Paige Bond, LMFT: That's what I'm thinking too, like you don't only have the stress of the chronic illness or condition, now you have the extra stress of not getting the basic needs met and then not having the emotional aspect. I would imagine that worsens conditions in a situation like that. Is that what you see?
Yeah, a lot of unfortunately, like that person isn't able to function as well or work. And maybe it might seem like a mystery to the partner, like "how come you're not doing more?" But as clinicians, we can see why not, if you're not feeling safe or supported, loved, basic needs are not being met. I mean, how can you function, you know what I mean? Like it takes a lot of bravery on like their part to come to therapy and work one-on-one to make sure that, they start understanding that there is help, that there is strength, that they hear messages, that they're not a burden, you know, to overcome the messages that unfortunately in their environment they're hearing, Yeah. I'm wondering in situations like this, like they're so delicate, especially when you're involving, Talking about and pointing out how you may have, hey, client and you have partner who's not being so supportive to you. is there a risk of damaging your rapport with this person that you're trying to kind of confront and say like, Hey, you're not getting the support you need out of this relationship when you told me you wanted X, Y, Z kind of support.
Like, has that ever gone wrong when you've been confronting them with what you observe and see?
[00:21:01] Jenelle Coolidge, LMHC: Yeah, it can be challenging because it's a delicate situation where it's Individual issues that they need to work on. But then there's also relationship issues. So sometimes if it gets too complex, it's like when I definitely be like, listen, I, I wanna send you some referrals for like couples counselors or something, to see a little bit more of that relationship dynamic because it I mean, it's playing a huge impact on your individual mental health. Like this isn't something that we can just leave it at here. You know? That's like when I'll definitely bring in that support,
[00:21:36] Paige Bond, LMFT: Yeah. And I, I don't know who you know who specializes in this. For me, I've had no training in like chronic illness.
I have had, some people that I've supported where like this is an aspect of their relationship, but not like an overarching theme why they're coming to therapy. So I'm wondering for you, like how hard is it to find, providers who can provide couples therapy, partnership therapy that specialize in chronic conditions?
Is that tough to find?
[00:22:07] Jenelle Coolidge, LMHC: Yeah, I can't think of somebody right now.
[00:22:11] Paige Bond, LMFT: Oh, that's so tough.
I have to do research. I mean, I guess we could like consult, you know, there's always consultations like right? The person has their individual therapist that knows about that, and then maybe they can collaborate with the couple's counselor, Yeah. So that would be a recommendation to have you or whoever the client is, the, the individual therapist of the person suffering from the chronic pain conditions collaborate with the couples therapists who might start seeing them with their partner.
[00:22:41] Jenelle Coolidge, LMHC: yeah. Yeah. I think that'd be, I think that's a good idea.
Definitely. Mm-hmm.
[00:22:46] Paige Bond, LMFT: I know I'm going all over the place here. I wanna go back to the, the idea of chronic fatigue. 'Cause fatigue- you know, we know like you're kind of like tired or drained, but what is the difference between chronic fatigue and being tired all the time? Because that sounds like too much of a generalization of being tired all the time to really pinpoint the specifics of the chronic fatigue condition.
So what is the difference?
[00:23:15] Jenelle Coolidge, LMHC: Yeah, and I could talk only from like my personal lived experience and what I've heard some clients. Say so, like before this, before this season of life, you know, I remember days like if I didn't sleep well, I stayed up too late, uh, feeling tired the next day, like, oh, I'm so sleepy, you know, I, I think I need a nap, or maybe I need to go to bed a little earlier. And, you know, after a couple days you, you're back to like your typical self, right? But just the shift that I notice is that sometimes it could appear like, kind of like when you have a cold or a flu, right? it's like a malaise throughout the whole body where it's not just, oh, you're, you tired.
No, it's like your whole body just feels like sluggish and moves slower and that is why it's sometimes mentally hard, because that can last a really long time for some people, especially if it's tied to a flare up. And that can just get really hard because sometimes other people might not understand.
Like, why are you moving slower? Why can't you socialize as much? Like, what's going on here? And even your personal frustration of like, oh, I wish I could just work more like others and, and do more. You know? It's that battle you're having with your body, you know?
[00:24:48] Paige Bond, LMFT: Yeah. I'm sure there's so many misconceptions that really, Dig at the insecurities that come up because of, its like, I can imagine people saying, or even like a boss saying like, you're just lazy. Like, why aren't you getting this done? Or something like that. I'm glad you used these words to describe it because I'm trying to imagine myself in full blown, like cold mode.
I don't wanna do anything. I just wanna lay in bed. I wanna recover and you know, watch some flicks on the TV or something, so I can't imagine trying to go through daily life and then just being told all of these negative messages that are, that eat at the insecurities that I'm already afraid of being seen.
So like within that, you mentioned self-compassion and self-care as part of some things that can help with these, aspects of dealing with these chronic conditions. Can you describe what that process might look like? The self-care or self-compassion?
[00:25:45] Jenelle Coolidge, LMHC: Yeah, absolutely. there's a couple of things like when people come to me that, I'm thinking about helping them work through, first of all, there is a lot of like working through the people pleasing tendencies of just keep saying yes and yes, even though your body needs rest.
So sometimes we have to work on that, right? And really prioritize what your body can do for the day. Really listening in so that you can give it what it needs. Like does it need a warm bath? Do you need, to do some stretches or yoga? Does this weekend need to be just lounging? Because I know we're in this hustle culture where it's like, we gotta be doing stuff every weekend all the time, and it's just like.
And you can't live like that. we can probably be all a little bit more balanced in life.
[00:26:43] Paige Bond, LMFT: I agree. I agree wholeheartedly.
[00:26:46] Jenelle Coolidge, LMHC: But it's extra important that these people living with a chronic condition are doing that extra self care, are making sure that sleep and nourishing their bodies.
taking time for themselves is a top priority, so that your body can just be strong, you know?
[00:27:07] Paige Bond, LMFT: Yeah. And then what would be the self-compassion aspect of it? some of the ways they may be talking to themselves to try to provide that kind of kindness that maybe they provide others but not so much themselves and need some improvement on.
[00:27:22] Jenelle Coolidge, LMHC: Absolutely. Yeah. Just coming back from the Body Kindness mentality, which is very similar to like body image work. we're looking at our body with like gratitude for what it can do today, and thanking it for trying. It's hard to sustain us, you know, our body is fighting for us. I mean, literally its job is to keep us alive and even if we're feeling a little sluggish just reminding about how amazing our body is and it's trying to keep us here and moving forward. And you just reminding yourself about that self-love can actually, really work on decreasing some symptoms. I mean that's why there's a lot of new techniques like somatic tracking from pain reprocessing theory that involves that whole sit in, listen to the body, and sense those sensations.
[00:28:26] Paige Bond, LMFT: Hmm. as you talk about how, this kind of can come from the body image work too. It does make me connect that, like of course we might start to see ourselves differently whenever our bodies may be transitioning into the level of work that we can put out because of whatever chronic condition that we're experiencing.
Or maybe we have certain limits or certain restrictions on what we can do, where we can go, what we can eat, whatever it may be. And I didn't even think about it until you, you were just saying it, how that can change the way that we see ourselves. And you're kind of blowing my mind in that this does go hand in hand.
the body image work, maybe eating disorder work and the chronic, like, I didn't understand that until you just talked about it just now. You're blowing my mind, Jenelle.
[00:29:19] Jenelle Coolidge, LMHC: Well, I appreciate it that I can blow mines.
[00:29:25] Paige Bond, LMFT: Of course you can. Yes.
[00:29:27] Jenelle Coolidge, LMHC: Yeah, it, this is why it's so common and it co-occur frequently, like chronic illness and an eating disorder.
You know, it just makes it so much more complex for that individual, you know, extra care going in there, a big, strong team of like dietician, therapists, medical doctors, psychiatrists, Physician, Support groups, you know, so they feel less alone.
It's like, you're not the only one experiencing this, even though it feels that way.
[00:30:03] Paige Bond, LMFT: Yeah.
[00:30:03] Jenelle Coolidge, LMHC: Whole community of people who are just wanting to live life together and support one another, you know?
[00:30:10] Paige Bond, LMFT: I hope you're enjoying this episode. I wanna take a moment to invite you to sign up for my free Attachment Dynamics workshop. I have partners use this as a foundation before we get started in relationship therapy.
By watching this, you'll learn how to recognize negative communication patterns, understand how power dynamics show up in conflict, and most importantly, discover ways to turn conflict into opportunities for deeper emotional connection. And the best part, this is free for you. Make sure to head to paigebond.com or hit the link in the show notes to access it for free.
Now let's get back to the episode.
[00:30:50] Paige Bond, LMFT: Now this is kind of going into a random place, but I'm wondering like, what do you think are some misconceptions about chronic illness, fatigue, pain, that you'd like to, bust some of those myths out there?
Are there any misconceptions that you hear of that aggravate you and grind your gears?
[00:31:10] Jenelle Coolidge, LMHC: Yeah, I would say kind of like the, maybe just more of the little phrases that people say. That don't mean to be, dismissive, but can be. Like for example, someone that lives with Crohn's, right?
IBS is very common, right? Irritable bowel syndrome from people don't know. And someone with IBS being like, oh yes, I know because like I have IBS and it's not like to take away from that person because IBS is very uncomfortable and does affect your day absolutely.
But when we're talking about someone living with this like disease, it kind of feels like you're not fully grasping what's going on here,
[00:31:57] Paige Bond, LMFT: Hmm.
[00:31:59] Jenelle Coolidge, LMHC: like, it's best if you just listen and be supportive, you know what I mean?
And even though if you don't understand, but you're there, whatever they may need.
[00:32:07] Paige Bond, LMFT: Yeah. It's like people showing up in a way where they downplay and minimize the gravity of What people who are suffering more intensely are going through when they say something like that.
[00:32:19] Jenelle Coolidge, LMHC: Yeah, that is exactly what it could feel like. It's kind of like, oh, Yeah, exactly. It's the downplaying of it, and then that person is already feeling downplayed and dismissed by the medical system. You know what I mean? So that's why it's extra sensitive, you know? I dunno a lot of chronic pain, chronic fatigue, like you said before, people might think that they're just being lazy or "what's wrong, are you depressed?" Maybe. Maybe 'cause they co-occur 'cause they have to self isolate. Yeah. I mean like, or that they are not, you know, people still wanna be. Invited to things because sometimes when people have chronic illness and pain, they have to say no to a lot of things and then that's when FOMO becomes even worse, right?
because, you know, the group of friends are like, oh, you know, they're not gonna wanna come 'cause they don't feel good. people don't wanna fe be feel forgotten because even if they're physical body can't allow 'em to do as much as they would like it, they still want company and support and check-ins.
And I've told clients of mine, 'cause some people have these really busy friend groups who like wanna do all this outdoor stuff, and it's like maybe having conversations with friends to meet you where you're at or like maybe go to the movies, maybe we watch movies at my house. kind of meeting them where they're at because people really do need support in community.
[00:33:53] Paige Bond, LMFT: I love those suggestions. Really talking about, "hey, these are my limits. What do we have in common that we could both, enjoy and have this shared interest over? I think too often we're just so selfish, naturally as humans and we think that there's only one way to do things or this is what I wanna do and we.
Don't realize that we have a lot more flexibility to still enjoy ourselves and, live our life by our values, but maybe tweak it a little bit differently based on, the people we love and still have a lot of fun and get a lot of joy out of it.
[00:34:30] Jenelle Coolidge, LMHC: Yeah, absolutely. I agree. There's different ways to show up for a friend and a loved one.
we can be more flexible.
[00:34:40] Paige Bond, LMFT: Yeah. this actually. Begs me to ask the question,how should people be going about checking in on loved ones who they know are struggling with chronic pain or illness? is it something that they even are allowed to ask? Is it taboo and, and disrespectful to check in on them of like, "Hey, is it a high pain day?"
Or, "Hey, how are you doing?" is it, something that like strikes a sensitivity in them and is considered disrespectful in a way. how should people approach this with their loved ones?
[00:35:14] Jenelle Coolidge, LMHC: Well, I do understand that there is probably a fine balance, or some people who are experiencing chronic conditions don't want to feel as like the sick one, you know what I mean? Yeah.
They don't want that identity, but I do think there is a way to communicate in a way where you're just Overall checking in, like emotionally because like most of us humans, no matter what we're going through, we all struggle and, and people with chronic illness are struggling heavily with their mental health.
And if you wanna make plans with the person, really listen to What feels comfortable for you? Like, what would you like it and being like, that's okay. That's fine with me. you wanna stay, do something indoors. That's okay. You know, I'm, I'm happy to be there and do that.
Kind of like that flexibility in there.
[00:36:12] Paige Bond, LMFT: Yeah. Yeah. Good. I'm trying to think, is there anything else that we haven't covered around this realm that you would really want listeners to know?
[00:36:23] Jenelle Coolidge, LMHC: Yeah, For a lot of people when they go see a lot of providers and are dealing with chronic pain and chronic health issues, sometimes they start to feel like they're so dismissed and invalidated and they're told that it's all in your head after a while.
[00:36:40] Paige Bond, LMFT: Yeah,
[00:36:41] Jenelle Coolidge, LMHC: and what I wanna say to that is that your pain and your fatigue is real if you're experiencing that. Yes. That I would agree to, to a certain point that, yeah, it is your brain sending you these signals of pain, but it's just like when it send signals of anxiety, Your brain just needs that extra love.
And what, what do we do for anxiety? We do mindfulness, we do deep breathing, we do relaxation. Those same techniques that you do for anxiety, you can do for pain and fatigue. And I, I have heard reports from clients including myself that, not that it zaps everything miraculously away, but there has been a decrease to the volume of the pain signals when you do those same type of techniques.
[00:37:39] Paige Bond, LMFT: Wow. Now that makes a difference. So if you're able to practice that mindfulness, you're saying that there could be a reduction in the intensity, someone might be feeling that pain. Yeah. That's, you hear listeners like, come on, let's take some breaths.
Let's go, let's do this. Let's, let's try to help you feel a little bit better. Yeah.
[00:38:01] Jenelle Coolidge, LMHC: They're together, mind and body. We cannot separate 'em.
[00:38:06] Paige Bond, LMFT: Yeah. Well I really love that you also have this medical background 'cause I think that flows so well. in the work that you do in all of these aspects.
It's so cool and interesting. thank you for sharing that. I definitely think we needed to hear it and be reminded of it if some of us knew about that, before. But yeah, definitely that mindfulness.
as we wind down and wrap up for this show, I want listeners to know, you know, if they wanna hear more about you, if they want to work with you, see what you got going on, can you point them in the right direction?
[00:38:39] Jenelle Coolidge, LMHC: Absolutely. You could find me on my website, www.coolskiescounseling.com, just like my practice, cool Skies counseling. You could also email me info@coolskiescounseling.com. I also have an Instagram called Cool case counseling as well.
[00:39:05] Paige Bond, LMFT: Good branding.
[00:39:06] Jenelle Coolidge, LMHC: You'll see. You can find me there. You can message me if you're interested in learning more. I also have a journal that I self publish. It's on Amazon. It's called My Body Liberation Journal. the intention was for body image, but like I said, like. When you work on body kindness or body gratitude, it can definitely still correlate with whatever you got going on with your body, you know?
[00:39:39] Paige Bond, LMFT: I love that. I'm so glad you plugged that in. so you're saying that even though that journal is more focused towards body image, it could still be very helpful for people dealing with chronic pain, chronic illnesses, because again, as we talked about today, they're so intertwined.
[00:39:54] Jenelle Coolidge, LMHC: Yeah, I definitely think it would make a big impact.
[00:39:57] Paige Bond, LMFT: Yeah. Beautiful.
thank you so much for taking your time today. I enjoyed having you on the show.
[00:40:03] Jenelle Coolidge, LMHC: Thank you for having me, Paige. It was really fun.
[00:40:05] Paige Bond, LMFT: Yeah. All right, listeners, I'm gonna have all Janelle's, links in the show notes wherever you're listening from so you can go check her out, check out our social media, go get her book and start practicing those mindfulness things.
All right, listeners. Until next time. Bye.
that's a wrap for today's episode of Stubborn Love. I hope you gathered some wisdom to bring into your love life and improve your relationships. If you enjoy today's chat, don't forget to subscribe and leave a review. That'll help this episode reach even more listeners. If you have any questions or stories you would like me to cover in the future episodes, drop me a message.
I love hearing from you. If you need extra support in your relationships, check out how we might be able to work together by hopping on my website @ paigebond.com. Until next time, don't let being stubborn keep you from secure love. Catch you in the next episode.